This is a handy reference for the typical questions which arise during the post-operative period, specifically related to the surgery you had. Most questions you may have will likely be answered here. However, if you feel you need to speak to the physician on call, you may call our office number 404-508-4320 at any time of the day or night. After hours, this phone number is forwarded to our automated answering service, which will typically connect you to the surgeon on call in just a minute or so, while you are still on the line. If the surgeon cannot take your call immediately, he will return your call, usually within about 20 minutes. If your call is not returned in 30 minutes, leave a second message. Of course, if you feel you may be having a life-threatening emergency, you should call 911 for immediate assistance.
General Instructions
If your operation isn’t listed above, here are some general post-operative instructions to follow.
Pain Medication
The medicine which was used may affect you for up to 24 hours after your procedure, so you might feel sleepy; this feeling will slowly wear off. BECAUSE THE MEDICINE MAY STILL BE IN YOUR SYSTEM FOR THE NEXT 24 HOURS, YOU SHOULD NOT:
- Drive a car or operate machinery or power tools
- Drink any alcoholic beverages
- Make any important decisions, such as signing important papers
A prescription for pain medication may be given by your physician. This should be taken as directed, and if the pain is not relieved, contact your physician. If your physician does not prescribe medication, you may take a non-prescription, non-aspirin medication which can be purchased at your drugstore. Please follow the directions on the label. Please be aware that any pain medication can affect your judgment.
The narcotic medications typically prescribed (eg, hydrocodone or oxycodone) can cause nausea, itching, or other side effects. It is best NOT to take these on an empty stomach. If you are nauseated or just not eating much yet, at least take a cracker along with this medication, to help lessen the possibility of worsening nausea. If you experience itching after taking one of these narcotic medications, it is likely due to an allergy to the medication. While in most cases, this is not severe, it is most likely best not to use even smaller doses of that specific narcotic in the future. You can use over the counter medications, such as Tylenol (acetaminophen), Aleve (naproxen), or Motrin or Advil (ibuprofen) instead, and in many cases, these options will be sufficient. But if not, call to report your problem, and an alternative choice will be given. And if you have experienced an allergic reaction, be sure to note the medication name, and add it to your written list of drug allergies and adverse effects.
Be aware that the narcotic medications (eg, hydrocodone (Lortab), oxycodone (Percocet)) usually include some acetaminophen. This improves the effect of the narcotic. Be aware that large daily total doses of acetaminophen can cause liver damage, so be sure to follow the instructions on the package or prescription.
Bandages
The use of ice packs is optional, but many patients find that it helps to lessen their pain, and speed up their recovery. Some swelling or bruising at the incision sites is normal.
Keep any clear plastic dressings on until your followup visit if possible.
You may take a brief shower leaving the clear dressings in place; do not soak in a tub bath.
Your dressings may become soaked or may leak. If so, you may remove the dressings and replace with dry gauze and adhesive tape daily. You may still gently shower and re-cover with gauze and tape afterward.
Dressings at the navel more often need to be replaced during the first week. If you note any drainage under the clear dressing, it may be best to replace sooner rather than later.
Diet
After general anesthesia, you may not have much appetite for the first 1-2 days after surgery.
Start with light foods (bread, bananas, soups) and advance as tolerated.
If you are nauseated, limit yourself to liquids until nausea resolves. If the nausea is your worst symptom, you may call the office phone number (404-508-4320) and ask for some medication to help with it.
Be aware that the pain medications prescribed, such as hydrocodone and oxycodone frequently cause constipation. If you are using these medications regularly for pain control, consider taking milk of magnesia once or twice daily to help prevent constipation from being a problem.
Driving
The main reason for restricting your driving is that your incisions will be sore, and you might not be able to put on the brakes comfortably enough to be a safe driver. Once you do this quickly and without pain, you may resume driving. But before getting out on the road, take a practice run just in your neighborhood.
Return to Work
In many cases, one can return to work in less than a week, but it does depend on what type of work you do, whether you have resumed driving as discussed above, and how much pain you are experiencing after surgery. If your job involves heavy lifting, or lots of standing and walking, your return to work could be delayed a bit longer. You can get a written work release and permission to return to work from the DeKalb Surgical office if needed.
Follow-Up Office Appointment
In most cases, your surgeon will want to see you back in the office in about one week, unless you have been instructed differently. You can call during regular office hours to make the appointment, using our main office phone number, 404-508-4320. Please be sure to make note in advance whether you have sufficient pain medication left, and if not, you can request a refill during your appointment. If there is any pathology report to go over, your surgeon should typically have it available by the time of the first visit. You may have a copy for your own records if requested. Prior to your appointment, it would be good to write down any questions you need answered, to be sure you don’t forget.
Breast Surgery
Pain Medication
The medicine which was used may affect you for up to 24 hours after your procedure, so you might feel sleepy; this feeling will slowly wear off. BECAUSE THE MEDICINE MAY STILL BE IN YOUR SYSTEM FOR THE NEXT 24 HOURS, YOU SHOULD NOT:
- Drive a car or operate machinery or power tools
- Drink any alcoholic beverages
- Make any important decisions, such as signing important papers
A prescription for pain medication may be given by your physician. This should be taken as directed, and if the pain is not relieved, contact your physician. If your physician does not prescribe medication, you may take a non-prescription, non-aspirin medication which can be purchased at your drugstore. Please follow the directions on the label. Please be aware that any pain medication can affect your judgment.
The narcotic medications typically prescribed (eg, hydrocodone or oxycodone) can cause nausea, itching, or other side effects. It is best NOT to take these on an empty stomach. If you are nauseated or just not eating much yet, at least take a cracker along with this medication, to help lessen the possibility of worsening nausea. If you experience itching after taking one of these narcotic medications, it is likely due to an allergy to the medication. While in most cases, this is not severe, it is most likely best not to use even smaller doses of that specific narcotic in the future. You can use over the counter medications, such as Tylenol (acetaminophen), Aleve (naproxen), or Motrin or Advil (ibuprofen) instead, and in many cases, these options will be sufficient. But if not, call to report your problem, and an alternative choice will be given. And if you have experienced an allergic reaction, be sure to note the medication name, and add it to your written list of drug allergies and adverse effects.
Be aware that the narcotic medications (eg, hydrocodone (Lortab), oxycodone (Percocet)) usually include some acetaminophen. This improves the effect of the narcotic. Be aware that large daily total doses of acetaminophen can cause liver damage, so be sure to follow the instructions on the package or prescription. Here is a link to more information about acetaminophen.
If you require additional narcotic pain medication, be aware that a written prescription is required by law. That means that a refill can NOT be transmitted electronically or by phone. You or someone for you, will need to come to the office to pick it up.
Bandages
You may place ice packs covered with a towel over the incision to decrease swelling during the first 24-48 hours after surgery. The use of ice packs is optional, but many patients find that it helps to lessen their pain, and speed up their recovery. Some swelling or bruising at the incision site is normal.
Keep any clear plastic dressings on until your followup visit if possible.
You may take a brief shower leaving the clear dressings in place; do not soak in a tub bath.
Your dressings may become soaked or may leak. If so, you may remove the dressings and replace with dry gauze and adhesive tape daily. You may still gently shower and re-cover with gauze and tape afterward.
If surgical glue is used, you may shower as long as there is no drainage from the incision. The glue will remain in place typically for a few weeks until it eventually peels off.
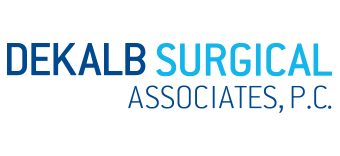
Drainage Tubes
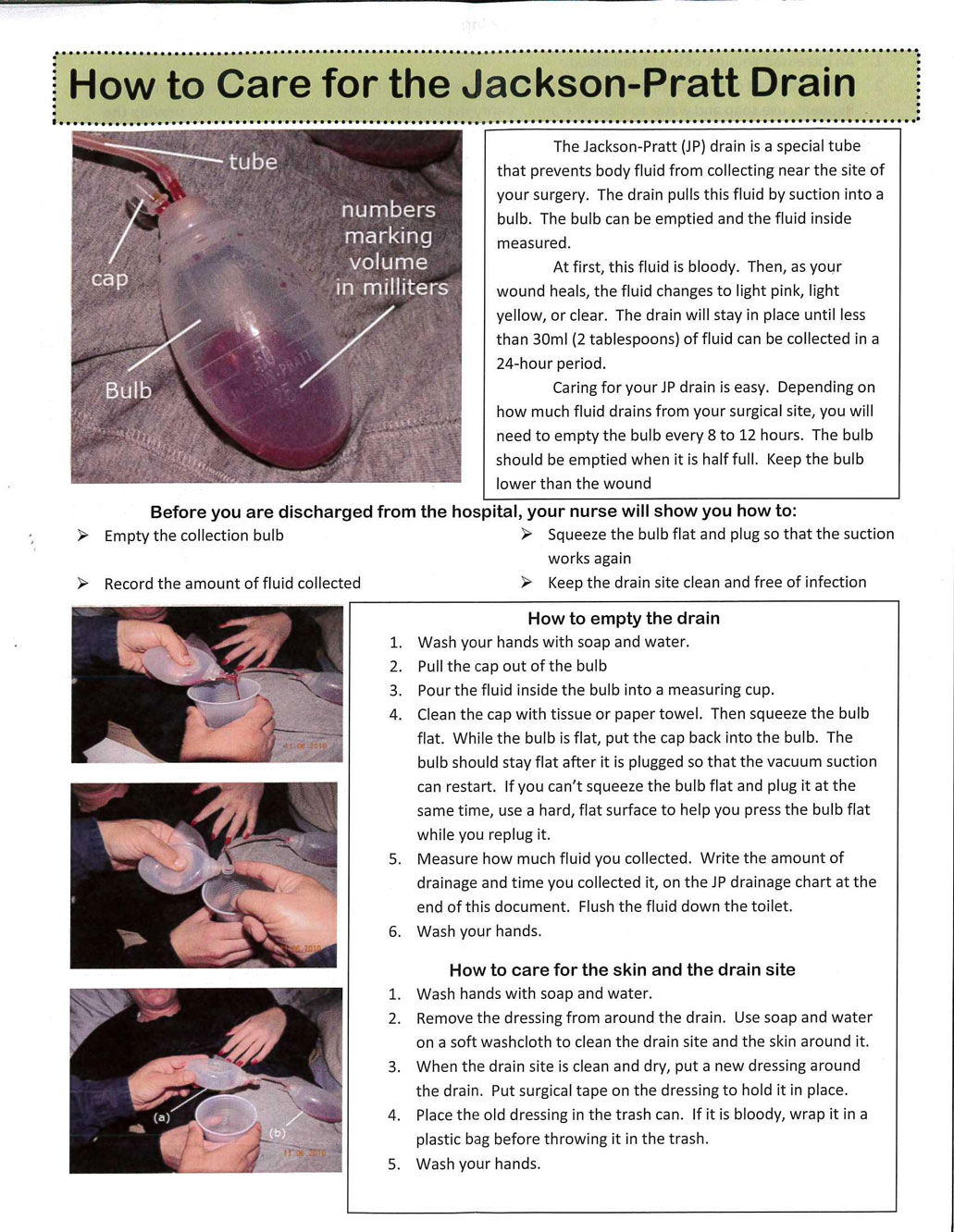
To keep the tubing open and free of a clot, it helps to “strip” the tubing anytime you empty the bulb. This is done by squeezing the tubing between your thumbnail and index finger, starting close to the body, stripping toward the bulb. Hold the tubing with your other hand close to the body, to prevent pulling the tubing out of the body. Repeat the stripping process until the tubing is slightly collapsed. You may see some thin strips of a blood clot in the tubing, and these should be “stripped” into the bulb.
There usually is very little drainage AROUND the tubing at the skin exit site. If you suddenly start seeing a lot of drainage AROUND the tubing, it may indicate that the tubing has become occluded. The instructions below explain how to change the dressing around your drain. But this is only necessary if there is enough drainage to saturate the dressings. If you note that there is little drainage into the bulb, but drainage saturating the dressings, call your doctor for instructions.
Diet
After general anesthesia, you may not have much appetite for the first 1-2 days after surgery.
Start with light foods (bread, bananas, soups) and advance as tolerated.
If you are nauseated, limit yourself to liquids until nausea resolves. If the nausea is your worst symptom, you may call the office phone number (404-508-4320) and ask for some medication to help with it.
Be aware that the pain medications prescribed, such as hydrocodone and oxycodone frequently cause constipation. If you are using these medications regularly for pain control, consider taking milk of magnesia once or twice daily to help prevent constipation from being a problem.
Driving
You can usually resume driving in just a day or two, but if you are still in a lot of pain, wait until it subsides.
Return to Work
In most cases, one can return to work in less than a week, but it does depend on what type of work you do, whether you have resumed driving as discussed above, and how much pain you are experiencing after surgery. You can get a written work release and permission to return to work from the DeKalb Surgical office if needed.
Follow-Up Office Appointment
In most cases, your surgeon will want to see you back in the office in about one week, unless you have been instructed differently. You can call during regular office hours to make the appointment, using our main office phone number, 404-508-4320. Please be sure to make note in advance whether you have sufficient pain medication left, and if not, you can request a refill during your appointment. If there is any pathology report to go over, your surgeon should typically have it available by the time of the first visit. You may have a copy for your own records if requested. Prior to your appointment, it would be good to write down any questions you need answered, to be sure you don’t forget. If you have a drain in place, be sure to bring the paper on which you have been recording the output, as this will help determine when the drain(s) can be removed.
Hernia Surgery
Pain Medication
The medicine which was used may affect you for up to 24 hours after your procedure, so you might feel sleepy; this feeling will slowly wear off. BECAUSE THE MEDICINE MAY STILL BE IN YOUR SYSTEM FOR THE NEXT 24 HOURS, YOU SHOULD NOT:
- Drive a car or operate machinery or power tools
- Drink any alcoholic beverages
- Make any important decisions, such as signing important papers
A prescription for pain medication may be given by your physician. This should be taken as directed, and if the pain is not relieved, contact your physician. If your physician does not prescribe medication, you may take a non-prescription, non-aspirin medication which can be purchased at your drugstore. Please follow the directions on the label. Please be aware that any pain medication can affect your judgment.
The narcotic medications typically prescribed (eg, hydrocodone or oxycodone) can cause nausea, itching, or other side effects. It is best NOT to take these on an empty stomach. If you are nauseated or just not eating much yet, at least take a cracker along with this medication, to help lessen the possibility of worsening nausea. If you experience itching after taking one of these narcotic medications, it is likely due to an allergy to the medication. While in most cases, this is not severe, it is most likely best not to use even smaller doses of that specific narcotic in the future. You can use over the counter medications, such as Tylenol (acetaminophen), Aleve (naproxen), or Motrin or Advil (ibuprofen) instead, and in many cases, these options will be sufficient. But if not, call to report your problem, and an alternative choice will be given. And if you have experienced an allergic reaction, be sure to note the medication name, and add it to your written list of drug allergies and adverse effects.
Be aware that the narcotic medications (eg, hydrocodone (Lortab), oxycodone (Percocet)) usually include some acetaminophen. This improves the effect of the narcotic. Be aware that large daily total doses of acetaminophen can cause liver damage, so be sure to follow the instructions on the package or prescription.
If you require additional narcotic pain medication, be aware that a written prescription is required by law. That means that a refill can NOT be transmitted electronically or by phone. You, or someone for you, will need to come to the office to pick it up.
Bandages
The use of ice packs is optional, but many patients find that it helps to lessen their pain, and speed up their recovery. Some swelling or bruising at the incision sites is normal.
Keep any clear plastic dressings on until your followup visit if possible.
You may take a brief shower leaving the clear dressings in place; do not soak in a tub bath.
Your dressings may become soaked or may leak. If so, you may remove the dressings and replace with dry gauze and adhesive tape daily. You may still gently shower and re-cover with gauze and tape afterward.
Dressings at the navel more often need to be replaced during the first week. If you note any drainage under the clear dressing, it may be best to replace sooner rather than later.
If surgical glue is used, you may shower as long as there is no drainage from the incision. The glue will remain in place typically for a few weeks until it eventually peels off.
Diet
Even if you have only had intravenous sedation and local anesthesia for your hernia repair, the medications used during the surgery might give you some nausea for a day or two. And after general anesthesia, you may not have much appetite for the first 1-2 days after surgery. But you may eat whatever appeals to you. If in doubt, liquids are generally a safer way to go.
Start with light foods (bread, bananas, soups) and advance as tolerated.
If you are nauseated, limit yourself to liquids until nausea resolves. If the nausea is your worst symptom, you may call the office phone number (404-508-4320) and ask for some medication to help with it.
Be aware that the pain medications prescribed, such as hydrocodone and oxycodone frequently cause constipation. If you are using these medications regularly for pain control, consider taking milk of magnesia once or twice daily to help prevent constipation from being a problem.
Driving
The main reason for restricting your driving is that your incisions will be sore, and you might not be able to put on the brakes comfortably enough to be a safe driver. Once you do this quickly and without pain, you may resume driving. But before getting out on the road, take a practice run just in your neighborhood.
Return to Work
In many cases, one can return to work in less than a week, but it does depend on what type of work you do, whether you have resumed driving as discussed above, and how much pain you are experiencing after surgery. If your job involves heavy lifting, or lots of standing and walking, your return to work could be delayed a bit longer. You can get a written work release and permission to return to work from the DeKalb Surgical office if needed.
Follow-Up Office Appointment
In most cases, your surgeon will want to see you back in the office in about one week, unless you have been instructed differently. You can call during regular office hours to make the appointment, using our main office phone number, 404-508-4320. Please be sure to make a note in advance whether you have sufficient pain medication left, and if not, you can request a refill during your appointment. If there is any pathology report to go over, your surgeon should typically have it available by the time of the first visit. You may have a copy for your own records if requested. Prior to your appointment, it would be good to write down any questions you need to be answered, to be sure you don’t forget.
Gallbladder Surgery
Pain Medication
The medicine which was used may affect you for up to 24 hours after your procedure, so you might feel sleepy; this feeling will slowly wear off. BECAUSE THE MEDICINE MAY STILL BE IN YOUR SYSTEM FOR THE NEXT 24 HOURS, YOU SHOULD NOT:
- Drive a car or operate machinery or power tools
- Drink any alcoholic beverages
- Make any important decisions, such as signing important papers
A prescription for pain medication may be given by your physician. This should be taken as directed, and if the pain is not relieved, contact your physician. If your physician does not prescribe medication, you may take a non-prescription, non-aspirin medication which can be purchased at your drugstore. Please follow the directions on the label. Please be aware that any pain medication can affect your judgment.
The narcotic medications typically prescribed (eg, hydrocodone or oxycodone) can cause nausea, itching, or other side effects. It is best NOT to take these on an empty stomach. If you are nauseated or just not eating much yet, at least take a cracker along with this medication, to help lessen the possibility of worsening nausea. If you experience itching after taking one of these narcotic medications, it is likely due to an allergy to the medication. While in most cases, this is not severe, it is most likely best not to use even smaller doses of that specific narcotic in the future. You can use over the counter medications, such as Tylenol (acetaminophen), Aleve (naproxen), or Motrin or Advil (ibuprofen) instead, and in many cases, these options will be sufficient. But if not, call to report your problem, and an alternative choice will be given. And if you have experienced an allergic reaction, be sure to note the medication name, and add it to your written list of drug allergies and adverse effects.
Be aware that the narcotic medications (eg, hydrocodone (Lortab), oxycodone (Percocet)) usually include some acetaminophen. This improves the effect of the narcotic. Be aware that large daily total doses of acetaminophen can cause liver damage, so be sure to follow the instructions on the package or prescription.
If you require additional narcotic pain medication, be aware that a written prescription is required by law. That means that a refill can NOT be transmitted electronically or by phone. You, or someone for you, will need to come to the office to pick it up.
Bandages
The use of ice packs is optional, but many patients find that it helps to lessen their pain, and speed up their recovery. Some swelling or bruising at the incision sites is normal.
Keep any clear plastic dressings on until your followup visit if possible.
You may take a brief shower leaving the clear dressings in place; do not soak in a tub bath.
Your dressings may become soaked or may leak. If so, you may remove the dressings and replace with dry gauze and adhesive tape daily. You may still gently shower and re-cover with gauze and tape afterward.
Dressings at the navel more often need to be replaced during the first week. If you note any drainage under the clear dressing, it may be best to replace sooner rather than later.
If surgical glue is used, you may shower as long as there is no drainage from the incision. The glue will remain in place typically for a few weeks until it eventually peels off.
Diet
Even if you have only had intravenous sedation and local anesthesia for your hernia repair, the medications used during the surgery might give you some nausea for a day or two. And after general anesthesia, you may not have much appetite for the first 1-2 days after surgery. But you may eat whatever appeals to you. If in doubt, liquids are generally a safer way to go.
Start with light foods (bread, bananas, soups) and advance as tolerated.
If you are nauseated, limit yourself to liquids until nausea resolves. If the nausea is your worst symptom, you may call the office phone number (404-508-4320) and ask for some medication to help with it.
Be aware that the pain medications prescribed, such as hydrocodone and oxycodone frequently cause constipation. If you are using these medications regularly for pain control, consider taking milk of magnesia once or twice daily to help prevent constipation from being a problem.
Driving
The main reason for restricting your driving is that your incisions will be sore, and you might not be able to put on the brakes comfortably enough to be a safe driver. Once you do this quickly and without pain, you may resume driving. But before getting out on the road, take a practice run just in your neighborhood.
Return to Work
In many cases, one can return to work in less than a week, but it does depend on what type of work you do, whether you have resumed driving as discussed above, and how much pain you are experiencing after surgery. If your job involves heavy lifting, or lots of standing and walking, your return to work could be delayed a bit longer. You can get a written work release and permission to return to work from the DeKalb Surgical office if needed.
Follow-Up Office Appointment
In most cases, your surgeon will want to see you back in the office in about one week, unless you have been instructed differently. You can call during regular office hours to make the appointment, using our main office phone number, 404-508-4320. Please be sure to make note in advance whether you have sufficient pain medication left, and if not, you can request a refill during your appointment. If there is any pathology report to go over, your surgeon should typically have it available by the time of the first visit. You may have a copy for your own records if requested. Prior to your appointment, it would be good to write down any questions you need answered, to be sure you don’t forget.
Parathyroid Surgery
What to Expect on the Day of Surgery and Afterward
You will be instructed to arrive a few hours before the scheduled start time for the surgery. After checking into the Surgical Admitting Center, your nurse will start an IV line. You will then be taken to the nuclear medicine Department for the sestamibi scan, to be done right before the surgery. Following this relatively short test, you will be taken back to the Surgical Admitting Center, and from there to the operating room. Your surgeon and the anesthesiologist will have discussed with you in advance the type of anesthesia to be utilized during the surgery.
When you wake up from the surgery, you probably will have some mild pain along the incision in your neck, and perhaps some soreness in your throat, depending on the type of anesthesia used. You might have hoarseness, but not to worry. If you are hoarse, it usually is related to the anesthesia effects, and should resolve over a few hours, sometimes, though, over a few days. You will still have an IV in your arm, but of course it will be removed before you leave. Following your recovery from anesthesia, you’ll be discharged from the hospital, usually in about 2 hours.
After the surgery is completed, your surgeon will talk with your family or whomever else accompanied you to the hospital. You’ll receive some postoperative instructions with plans for followup, and probably some instructions regarding taking calcium and vitamin D daily.
How Long Will It Take for My Symptoms to Go Away?
The symptoms that can be associated with a high calcium level are discussed elsewhere in this website. You can expect some fairly quick relief of the musculoskeletal types of symptoms you might be suffering from if they are due to the high calcium level. Other symptoms such as memory problems, concentration problems, headaches, and irritability typically improve over the first week or two. If you are having reflux symptoms related to a high calcium level, you are likely to see some dramatic improvement in the very first day or so. Symptoms of depression may take a month or two to improve. I wish I could guarantee that everyone with any of the listed symptoms will see dramatic improvement, but there is no guarantee of this. Fortunately, many patients do experience at least partial and often dramatic relief of their symptoms.
How Soon Will My Calcium Level Be Normal?
Patients with hyperparathyroidism don’t process calcium properly. The elevated PTH level stimulates your bones to release calcium, rather than store calcium, so until the elevated PTH level is corrected with a successful operation, your bones won’t be able to properly maintain their own health. Immediately after the surgery, your PTH level will drop to normal, and in fact, until your other (normal) parathyroid glands get “revved up” again, your body might have trouble keeping your blood calcium level high enough. This is just temporary, though, and once your PTH level comes back to normal levels, your bones can start storing calcium again like they should.
Calcium supplements can ensure your body has enough calcium to restore the deficit in your bones. Temporarily, we usually suggest above normal dosages of calcium (and vitamin D) to counteract this effect. Calcium can be taken in a variety of ways. Good food sources of calcium include dark green leafy vegetables (like spinach), cheeses, salmon, ice cream, calcium-fortified orange juice, and calcium-fortified cereals. A glass of milk (300 mg) is another option. If you don’t have any calcium tablets at home, you may want to get them from your pharmacy before your surgery so you can start taking them as directed right away. You will receive specific instructions about this, usually taking a few 600 mg tablets twice a day for a week, then decreasing to 2 tablets once daily, to continue as a maintenance dose. Particularly for women, those with or without hyperparathyroidism, this is usually thought to be a good idea to ensure your calcium intake is adequate for good bone health, and for prevention (or as part of the treatment for) osteoporosis.
There are a few options for calcium supplementation, including calcium by itself (either as calcium carbonate, calcium citrate, or calcium gluconate), or any of these combined with vitamin D. You do not need a prescription for calcium tablets. Calcium carbonate supplements (includes OsCal, Rolaids, and Tums) are usually the least expensive and well tolerated. But if you are on a drug which decreases stomach acid(for example, Pepcid, Zantac, Protonix, Nexium, Axid, or similar “H2 blockers” or “proton pump inhibitors”), calcium citrate (CitriCal) is probably a better choice, because of better absorption. The supplements with vitamin D are often recommended as an added margin of safety to ensure adequate vitamin D levels since this vitamin is necessary for the metabolism of calcium in the body. This is not necessary for everyone, but essentially safe for anyone, so you may as well use these. Most women, even without a parathyroid problem, should take a calcium supplement daily. If you have some tingling even with this dose, then you should take some more. Occasionally a patient might need as much as 10 grams of calcium (that’s almost 20 tablets!) temporarily to get rid of the symptoms.
Once the normal glands kick in, your calcium level will be maintained in the normal range without the need for supplements. If you are still having some tingling symptoms in your hands or around your mouth even with some extra tablets, you should call the DeKalb Surgical office (404-508-4320). On occasion, a patient might be sent to the hospital for some calcium by vein, though this is not often necessary.
Pain Medication
The medicine which was used may affect you for up to 24 hours after your procedure, so you might feel sleepy; this feeling will slowly wear off.
BECAUSE THE MEDICINE MAY STILL BE IN YOUR SYSTEM FOR THE NEXT 24 HOURS, YOU SHOULD NOT:
- Drive a car or operate machinery or power tools
- Drink any alcoholic beverages
- Make any important decisions, such as signing important papers
A prescription for pain medication may be given by your physician. This should be taken as directed, and if the pain is not relieved, contact your physician. If your physician does not prescribe medication, you may take a non-prescription, non-aspirin medication which can be purchased at your drugstore. Please follow the directions on the label. Please be aware that any pain medication can affect your judgment.
The narcotic medications typically prescribed (eg, hydrocodone or oxycodone) can cause nausea, itching, or other side effects. It is best NOT to take these on an empty stomach. If you are nauseated or just not eating much yet, at least take a cracker along with this medication, to help lessen the possibility of worsening nausea. If you experience itching after taking one of these narcotic medications, it is likely due to an allergy to the medication. While in most cases, this is not severe, it is most likely best not to use even smaller doses of that specific narcotic in the future. You can use over the counter medications, such as Tylenol (acetaminophen), Aleve (naproxen), or Motrin or Advil (ibuprofen) instead, and in many cases, these options will be sufficient. But if not, call to report your problem, and an alternative choice will be given. And if you have experienced an allergic reaction, be sure to note the medication name, and add it to your written list of drug allergies and adverse effects.
Be aware that the narcotic medications (e.g., hydrocodone (Lortab), oxycodone (Percocet)) usually include some acetaminophen. This improves the effect of the narcotic. Be aware that large daily total doses of acetaminophen can cause liver damage, so be sure to follow the instructions on the package or prescription. If you require additional narcotic pain medication, be aware that a written prescription is required by law. That means that a refill CANNOT be transmitted electronically or by phone. You or someone for you, will need to come to the office to pick it up.
Bandages
The use of ice packs is optional, but many patients find that it helps to lessen their pain, and speed up their recovery. Some swelling or bruising at the incision sites is normal. Keep any clear plastic dressings on until your followup visit if possible. If “surgical glue” is used, you don’t need any additional dressing and you may bathe normally. You may take a brief shower leaving the clear dressings in place; do not soak in a tub bath. Your dressings may become soaked or may leak. If so, you may remove the dressings and replace with dry gauze and adhesive tape daily. You may still gently shower and re-cover with gauze and tape afterward.
If surgical glue is used, you may shower as long as there is no drainage from the incision. The glue will remain in place typically for a few weeks until it eventually peels off.
Diet
After general anesthesia, you may not have much appetite for the first 1-2 days after surgery. Start with light foods (bread, bananas, soups) and advance as tolerated. If you are nauseated, limit yourself to liquids until nausea resolves. If the nausea is your worst symptom, you may call the office phone number (404-508-4320) and ask for some medication to help with it. Be aware that the pain medications prescribed, such as hydrocodone and oxycodone frequently cause constipation. If you are using these medications regularly for pain control, consider taking milk of magnesia once or twice daily to help prevent constipation from being a problem.
Driving
The main reason for restricting your driving is that your incisions will be sore, and you might not be able to put on the brakes comfortably enough to be a safe driver. Once you do this quickly and without pain, you may resume driving. But before getting out on the road, take a practice run just in your neighborhood.
Return to Work
In many cases, one can return to work in less than a week, but it does depend on what type of work you do, whether you have resumed driving as discussed above, and how much pain you are experiencing after surgery. If your job involves heavy lifting, or lots of standing and walking, your return to work could be delayed a bit longer. You can get a written work release and permission to return to work from the DeKalb Surgical office if needed.
Follow-Up Office Appointment
In most cases, your surgeon will want to see you back in the office in about one week, unless you have been instructed differently. You can call during regular office hours to make the appointment, using our main office phone number, 404-508-4320. Please be sure to make note in advance whether you have sufficient pain medication left, and if not, you can request a refill during your appointment. If there is any pathology report to go over, your surgeon should typically have it available by the time of the first visit. You may have a copy for your own records if requested. Prior to your appointment, it would be good to write down any questions you need answered, to be sure you don’t forget.
Wound Care Instructions for Minor Office Procedures
Dressing
In most cases, a clear (Tegaderm) dressing will have been placed over your incision. This is intended to be “maintenance free”, and does not need to be changed unless it becomes saturated. You can leave this original dressing on for anywhere from 2-7 days, then simply remove it.
If the dressing becomes saturated, you should remove it and apply some alternative dressing. Plain gauze dressing can be purchased from your pharmacy. Paper tape seems to be the best choice to secure it. If you need to change the original dressing, you may change your dressing once daily, or more often if needed. If there is continued oozing from the incision, call our office.
Packing
If you have any sort of infection which was drained or opened, your surgeon may have placed some packing gauze called iodoform. In this case, you will likely be instructed to change the dressing as needed, usually once daily. Be careful to avoid pulling the iodoform gauze out when the dressing is changed. If it does come out, that’s usually okay, and your surgeon can replace it at your follow-up visit if needed.
Your surgeon may give you some instructions on changing the packing at home as well.
Showers/Bathing
If the original Tegaderm dressing stays intact, in most cases you may shower, and just let the water run off the dressing. Gently pat the dressing dry, and it should stay in place. If it does get wet, you may remove it. If there is still any drainage, simply apply an alternative dressing as described above.
If you have a different type of dressing which is not water resistant, you’ll need to keep it dry initially. Your surgeon should specify when you may shower.
Pain Medication
Most office procedures do not cause much pain, and if you need something, usually an over-the-counter medication such as Tylenol, Aleve, Motrin, or similar product can be used. We discourage aspirin-containing products, as they can increase the possibility of oozing through the incision. But if you are on aspirin on a regular basis because of underlying heart disease, in most cases you can continue this. Your surgeon may have given you a prescription for something stronger if he thinks it might be necessary, and you can use this according to the instructions. You should not take more than 12 Tylenol or acetaminophen pills in any 24-hour period. Be aware that some prescription medications also include acetaminophen.
Activities
Depending on where your incision is, you may or may not resume usual activities. Common sense will go a long way in making your own decisions about specific activities. If an incision is near a joint, such as your shoulder, you should limit the motion of that joint. This will help decrease any pain you might have, and will facilitate proper healing.
Some swelling, redness, and pain are common with all wounds and normally will go away as the wound heals. If swelling, redness, or pain increases f the wound feels warm to the touch, or if the wound edges reopen or separate, call our office at 404 508-4320.