Hemorrhoids, or piles, are a sometimes painful mass of distended (swollen) veins in the lining of the anus and rectum, resulting from the formation of varicose veins around the anus. Internal hemorrhoids occur at the junction of the anus and rectum and are covered with mucous membrane. External hemorrhoids occur just outside the anus and are covered with skin. On occasion, internal hemorrhoids may prolapse, or protrude, to the outside, cutting off the blood supply. A number of treatments are available for internal hemorrhoids. External hemorrhoids may be treated with local care to relieve pain; if they recur or remain symptomatic they may be surgically removed.
Hemorrhoids can occur at any age, often without apparent cause. A typical scenario for developing hemorrhoids might be someone with a little chronic constipation, who sits for several minutes or more for each bowel movement, often reading a magazine or newspaper at the same time. Repeated straining at stool, over time, causes the encircling dilated veins to gradually stretch and get pushed downward through the anus, ahead of the stool. You might notice that you must wipe several times afterward, and you may be aware of some “extra tissue” protruding through the anus, or note a little trace of blood on the toilet paper. Contributing factors may include severe constipation or diarrhea, pregnancy, liver disorders, rectal tumors, and the repeated long-term use of laxatives. Hemorrhoids can cause itching and burning and may bleed during a bowel movement.
Hemorrhoids do not cause cancer nor do they become cancerous. But any rectal bleeding may be a sign of cancer of the colon or rectum and should be checked by a physician.
Temporary relief from hemorrhoids may be obtained by applying a cold compress directly to the affected area until the pain subsides. This is most easily done if the patient lies face-down and another person applies the compress. Tepid water baths may also help. A person should eat a high-roughage diet to ensure regular defecation of large, soft stools. Ointments, creams, and suppositories containing corticosteroids may also ease the symptoms. In addition to these measures, avoiding constipation is certainly key. It is important to have an adequate amount of fiber in your daily diet. So what do we mean by that? Well, the short answer is to have some sort of bran cereal for breakfast, like All Bran (probably the highest fiber content of the options available), or Raisin Bran, then be sure to include salads and lots of fresh fruits and vegetables in your other meals. You should also drink 6-8 glasses of water or juices per day. Lots of fiber without enough fluids can make the situation worse, similar to the difference between a dry and a wet sponge. The fiber (sponge) can absorb lots of liquid, but without the liquid, the stool will be hard to pass (like a dry sponge).
There’s more detailed information about fiber in the next few paragraphs.
Dietary fiber or roughage is defined as a carbohydrate complex which comes from plants, and it does not get digested in the stomach and small intestine. Since it remains in this undigested state all the way to the colon (large intestine), the remaining fiber absorbs water into the stool, creating bulk and speeds the process by which waste is eliminated from the body.
There are two types of fiber:
Although dietary fiber has little nutritional value, it has great health benefits. Everyone should be aware of how it can help you lead a healthier life:
Recommended daily amounts of fiber needed by adults according to the National Academy of Sciences’ Institute of Medicine:
| Ages 50 and Younger | Ages 51 and Older | |
|---|---|---|
| Men | 38 grams | 30 grams |
| Women | 25 grams | 21 grams |
Adding more dietary fiber to your meals is one of the nicest things you can do for yourself. If you have hemorrhoids, fiber can work to aid your digestive system in healing and eliminating them.
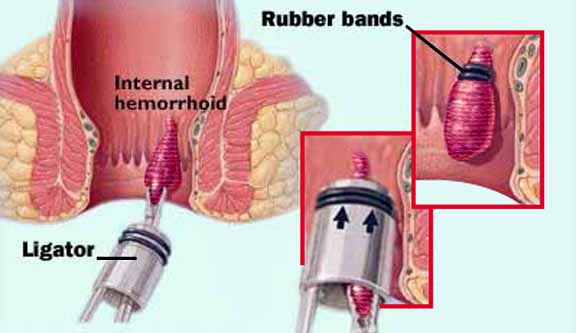
All cases of rectal bleeding should be examined by a physician to rule out the cancer of the colon and rectum. If the diagnosis is hemorrhoids, the remedies mentioned above may solve the problem. However, persistent hemorrhoids may need to be removed, using one of several methods. Hemorrhoids may be frozen off during cryosurgery; hardened, using a sclerosing agent; tied off, using a rubber band at the base of hemorrhoid; or removed surgically (hemorrhoidectomy). At DeKalb Surgical, the preferred method for most symptomatic hemorrhoids is the rubber band technique, which can be performed as an office procedure.
Hemorrhoids are typically classified according to the amount of prolapse (sticking out) that occurs. Those hemorrhoids which do not prolapse, or which spontaneously reduce (go back inside the anus) can usually be treated in the office setting. At DeKalb Surgical Associates, rubber band ligation is most often used. These small bands are placed over the hemorrhoid tissue, causing them to slowly strangulate and fall off. This treatment can be repeated if necessary. Though some patients experience moderate pain, in most cases, the procedure is tolerated with little discomfort.
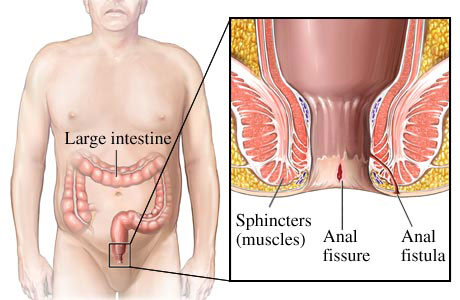
A fistula is an abnormal channel from a hollow body cavity to the surface (for example, from the rectum to the skin) or from one cavity to another (for example, from the vagina to the bladder). A fistula may be congenital (bladder to navel), the result of a penetrating wound (skin to the lung), or formed from an ulcer or an abscess (appendix abscess to the vagina, or tooth socket to sinus).
The repeated filling of an abscess or a wound by the fluid contents of some body cavities prevents healing and encourages the formation of a fistula. An anal fistula, for example, begins with inflammation of the mucous lining of the rectum. The area becomes an abscess as it is constantly reinfected by feces; eventually, a fistula breaks through the skin near the anus. The usual treatment is an operation to open the fistula channel completely and drain any abscess so it does not recur.
Anal fissures are small tears in the mucus lining of the anal canal. They can occur as a result of the passage of a large hard stool. Fissures can be quite painful, particularly with bowel movements. Often, some bright red blood will be noticed on the stool, or on the toilet paper after wiping.
If you have ever had a painful papercut on your finger, you can understand all about anal fissures. The anus is the ring-like sphincter or valve at the end of your rectum. It relaxes and tightens at your will to allow a bowel movement when convenient. An anal fissure is a small tear in the rim of the anus – just like a tiny papercut.
One problem with a papercut is that every time you use your hands, you tend to break open the small wound, which delays healing and causes more pain. The same holds true with an anal fissure. Every time you have a bowel movement, the anus is stretched and the fissure can possibly be reopened causing more symptoms. This makes some anal fissures chronic and difficult to heal. This problem is quite common and may cause considerable misery.
Fissures will often heal on their own if constipation is avoided. There are some simple measures that can be used to hasten the healing, including the use of stool softeners, and ointments such as Preparation H. Prescription medications may also be used, including a variety of analgesics, and steroid preparations. A more recent treatment option is the use of nitroglycerin ointment, the same type of medication used for patients with angina (heart pain). This medication relaxes the smooth muscle lining underneath the torn mucus layer of the anus. By treating the spasm of this smooth muscle, the fissure will heal in about 85% of cases. However, many patients have headaches as a result of using the nitroglycerin (because it relaxes smooth muscle cells in the arteries to the brain as well).
If the fissure does not heal, a simple outpatient surgical technique, called a lateral internal sphincterotomy, can be used.
The anal canal is anesthetized by injection with a small needle. A small incision is made in the anal canal, and the ring of muscle under the fissure is cut. This relieves the muscle spasm, which in turn allows the fissure to heal. Patients often experience an immediate improvement in their symptoms, though in some cases, the improvement is slower. Potential side effects or complications include temporary incontinence, bleeding, or persistent pain. Incontinence as a complication is unusual, but there may be temporary difficulty in distinguishing between gas, liquid stool, or solid stool in the rectum.
The anal opening is only so big. To have a bowel movement the anal sphincter relaxes and open up as much as it can, but the stool must still be soft enough to squeeze through the opening. If the stool is dry and hard, the anal sphincter is forced to open even wider than normal. This difficult passage can cause a tear in the rim of the anal opening, resulting in a fissure. Other causes of a fissure include severe diarrhea, inflammatory bowel disease, and sexually related trauma.
Fissures are graded as superficial or deep. A superficial fissure does not extend full thickness through the skin; a deep fissure results in exposing underlying muscle fiber. Fissures are also graded as acute or chronic. An acute fissure is less than thirty days duration; a chronic fissure is present for greater than thirty days.
Once the skin is torn, each subsequent bowel movement can be painful. Just like a papercut, it doesn’t take a very big tear to cause considerable misery. The pain is often quite severe. Patients often complain of a stinging pain during bowel movements. The pain often lasts for hours and gradually subsides. This occurs with each bowel movement. Many times there is also some bleeding on the toilet paper, which is usually of small quantity and generally bright red in color. The symptoms of an anal fissure are commonly mistaken for hemorrhoids, but hemorrhoids generally do not cause pain with bowel movements. In chronic cases, there may be the development of a localized swelling called a sentinel pile. This is commonly mistaken for a hemorrhoid.
An accurate diagnosis is the first step in treatment. Your doctor can perform special tests to be certain about the cause of your symptoms. This will include an examination of the anus and anal canal in the office. The tear of the skin is usually easy to visualize, although sometimes the pain precludes an adequate exam without anesthesia. Occasionally a small viewing instrument called an anoscope, is used in the evaluation. To rule out other more serious possibilities, a flexible sigmoidoscopy or full colonoscopy examination may be recommended.
If you could not use your anus for a few weeks, the fissure would probably heal faster, but, of course, you have to eat… and eliminate. Fortunately, over half of fissures heal either by themselves or with non-surgical treatment in a few weeks or months. Superficial fissures rarely require surgery; most are able to be treated with topical medications. Non-surgical treatments may include:
Call your doctor if you have any severe bleeding or fever, or if the fissure becomes more painful or shows no improvement after 3 days of treatment.
Two new forms of treatment have recently been reported. One is the use of Nitroglycerine cream to the anal area to relax the anal muscle spasm. Though frequently effective, many patients experience headaches when using this ointment. The other new treatment is the use of Botox (botulism toxin) injections to weaken the anal sphincter and allow the fissure to heal. Experience with this novel technique is limited.
If a fissure continues to cause pain and bleeding and does not respond to conservative medical therapy, it is considered chronic and surgery may be required. Chronic fissures heal only 10% of the time without surgery. This may involve an operation that divides one of the circular anal muscles (internal lateral sphincterotomy). Surgery can usually be performed without an overnight hospital stay. The pain often disappears a few days after surgery, though full healing requires one to two months Most patients are back to normal activity within a week or two.
There is a risk of fecal incontinence (loss of the ability to control bowel movements) with this procedure, but the incidence of this is quite low. Infection and complications incident to anesthesia are also possible, but again the risks are low. If you have any questions about this, you should discuss them with your doctor.
More than 90% of patients who require surgery for this problem have no further trouble from fissures as long as they take measures to prevent constipation and straining with bowel movements.